399,99 €
Mehr erfahren.
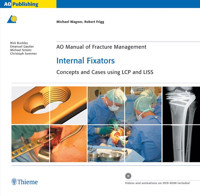
- Herausgeber: Thieme
- Kategorie: Fachliteratur
- Sprache: Englisch
Includes interactive CD-ROM!
This is the first compendium of principles of using locking compression plates in fracture management. With more than 100 cases from world-leading surgeons, including the inventors of the technique, this book will guide orthopedic trauma surgeons, general orthopedists, and residents through applications of the internal fixator technique. Intraoperative photos and illustrations and an interactive DVD containing additional cases, animations, and videos make this AO Manual an indispensable reference.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 918
Veröffentlichungsjahr: 2006
Ähnliche
AO Manual of Fracture Management
Michael Wagner, Robert Frigg
Internal Fixators
Concepts and Cases using LCP and LISS
800 illustrations, 2280 pictures and x-rays117 step-by-step case descriptions
Illustrations: tadpole GmbH, CH-8048 Zürich
DVD-ROM programming: interaktion GmbH, CH-8330 Pfäffikon
Library of Congress Cataloging-in-Publication Data is available from the publisher.
Hazards
Great care has been taken to maintain the accuracy of the information contained in this publication. However, the publisher, and/or the distributor, and/or the editors, and/or the authors cannot be held responsible for errors or any consequences arising from the use of the information contained in this publication. Contributions published under the name of individual authors are statements and opinions solely of said authors and not of the publisher, and/or the distributor, and/or the AO Group.
The products, procedures, and therapies described in this work are hazardous and are therefore only to be applied by certified and trained medical professionals in environments specially designed for such procedures. No suggested test or procedure should be carried out unless, in the user's professional judgment, its risk is justified. Whoever applies products, procedures, and therapies shown or described in this work will do this at their own risk. Because of rapid advances in the medical sciences, AO recommends that independent verification of diagnosis, therapies, drugs, dosages, and operation methods should be made before any action is taken.
Although all advertising material which may be inserted into the work is expected to conform to ethical (medical) standards, inclusion in this publication does not constitute a guarantee or endorsement by the publisher regarding quality or value of such product or of the claims made of it by its manufacturer.
Legal restrictions
This work was produced by AO Publishing, Davos, Switzerland. All rights reserved by AO Publishing. This publication, including all parts thereof, is legally protected by copyright. Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher's consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc. referred to in this publication are also protected by patents and trademarks or by other intellectual property protection laws (eg, “AO”, “ASIF”, “AO/ASIF”, “TRIANGLE/GLOBE Logo” are registered trademarks) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc. without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Publishing, Switzerland”.
Copyright © 2006 by AO Publishing, Switzerland, Clavadelerstrasse 8, CH-7270 Davos PlatzDistribution by Georg Thieme Verlag, Rüdigerstrasse 14, DE-70469 Stuttgart andThieme New York, 333 Seventh Avenue, New York, NY 10001, USA
Rest of WorldISBN 978-3-13-143551-4
The AmericasISBN 978-1-58890-486-7
2 3 4 5 6
Table of contents
Concepts
1 Background and methodological principles
1 Osteosynthesis
2 Concepts of fracture fixation
3 Mechanical aspects of plate and screw fixation
4 Development of internal fixators
5 Methods and techniques in plate osteosynthesis
6 Minimally invasive plate osteosynthesis (MIPO)
7 Bibliography
2 Surgical reduction techniques
1 Aim of reduction
2 Different types of surgical reduction
3 Instruments and techniques
4 Assessment of reduction
5 Conclusions
6 Bibliography
3 Techniques and procedures in LISS and LCP
1 The less invasive stabilization system (LISS)
2 The locking compression plate (LCP)
3 Bibliography
4 Pitfalls and complications
1 Implant-related problems
2 Technical errors
3 Pitfalls and complications during rehabilitation
4 Suggestions for further reading
Cases
5 Shoulder girdle
5.1 Clavicle
5.2 Scapula
6 Humerus
6.1 Humerus, proximal
6.2 Humerus, shaft
6.3 Humerus, distal
7 Radius and ulna
7.1 Radius and ulna, proximal
7.2 Radius and ulna, shaft
7.3 Radius and ulna, distal
8 Pelvic ring and acetabulum
8.1 Pelvic ring and acetabulum
9 Femur
9.1 Femur, proximal
9.2 Femur, shaft
9.3 Femur, distal
10 Tibia and fibula
10.1 Tibia and fibula, proximal
10.2 Tibia and fibula, shaft
10.3 Tibia and fibula, distal
11 Calcaneus
11.1 Calcaneus
To access additional material available for this e-book, please go to MediaCenter.thieme.com. You will be asked to login to this site using your thieme.com account credentials. If you don't have a thieme.com account, please register first. Click on “All titles” at the top of the page to find the additional material for your e-book and enter the following access code to gain access: EUSX-M4D8-A9X5-QGM8
Forewords
Thomas P Rüedi
For almost 40 years AO compression plate fixation providing absolute stability—as introduced by Maurice Müller—was the gold standard in operative fracture treatment. In the 1980s the locking intramedullary nail opened up new perspectives for the stabilization of diaphyseal fractures. As an internal splint this device provides relative stability, which allows rapid fracture healing with abundant callus formation. Perren and Tepic showed in the early nineties that, thanks to locking head screws (LHS) providing angular stability, the longitudinal stabilizer, eg, a plate could be kept at a distance from the bone similar to the external fixator and without interfering with periosteal or cortical vascularity. This innovative, quite different and biologically gentle as well as less invasive fixation principle was called “internal fixation”. Clinically, it was applied as the PC-Fix (point contact fixator) and LISS (less invasive stabilization system).
The actual breakthrough for the new internal fixator principle occurred however, when Michael Wagner as clinician, together with the engineer Robert Frigg, designed and developed the so-called “combination hole”. The idea and new design of the screw hole—a combination of the dynamic compression unit for standard cortex screws with a threaded hole for the LHS—could be introduced in any of the existing plates and required only a few additional instruments. The new and very versatile locking compression plate system—LCP—with its three different possibilities of applications and functions found immediately wide acceptance and has revolutionized operative fracture fixation in a similar way to the original compression plate and twenty years later the interlocking in-tramedullary nail.
It seemed therefore logical that Michael Wagner should also pioneer the collection of LCP and LISS cases for a book that addresses not only the basic principles, attributes, and different applications of the new implants but also highlights the pearls and pitfalls of the internal fixators in the clinic. Together with the contributions of other enthusiastic but also critical users the authors share experiences with these devices and gives valuable, practical recommendations to newcomers. The best stabilization system is of little use if the vascularity of the soft as well as hard tissues are not carefully respected. An entire chapter has therefore been dedicated to the most difficult and demanding challenges of any fracture treatment—the fracture reduction.
The editors, Michael Wagner and Robert Frigg, and the coauthors have to be complimented for a most comprehensive and attractive book on the clinical applications of the new internal fixator principles with the LISS and LCP, which are introducing interesting possibilities and opportunities especially in articular fractures as well as providing new hopes for severely osteoporotic patients.
The team at AO Publishing has again displayed its ability to produce, together with Thieme Verlag, a most attractive book that will find numerous readers and thereby help to improve patient care.
Thomas P Rüedi, MD, FACSFounding Member of the AO FoundationDavos, April 2006
Stephan M Perren
Fracture treatment has undergone a fascinating evolution. Early in the last century the main goal of treatment was to reach solid union. Then stable fixation and functional postoperative treatment successfully eliminated fracture disease. Now we can take advantage of restoring function while inducing prompt and safe healing and reducing the risk of biological complications.
In the early days the excessive external immobilization of the neighboring articulations too often resulted in damage to the articulations and even worse to the soft tissues and blood supply. In my own “pre AO” experience I observed a high incidence of what was later called fracture disease (Sudeck's or reflex dystrophy). Swelling, pain, patchy bone loss, and stiff articulations were accepted as the natural consequence of fracture. It is interesting to note that each generation was (and is!) blinded by the “state-of-the-art”.
In the late fifties the visionary Maurice E Müller and his colleagues effected a worldwide change in the fight against fracture disease. They studied and advocated precise reduction and compression fixation so that fracture healing could take place in a mechanically neutral environment. Dystrophy became a very rare incident and fracture healing showed a fascinating histology: direct healing. The price paid for focusing on mechanical advantages was that this approach did not induce early healing and so implants could not be removed earlier than one to two years postoperatively. This was not a major problem in view of the fact that the implants were mechanically protecting the fracture. Still, the observation of late union was a strong indicator that there was room for improvement. Considerable damage to the soft tissues and blood supply to bone in the hands of the less experienced resulted in complications due to a disregard for biology.
The promoters of stable internal fixation had to face harsh criticism, mainly focused on the complications of such treatment like infections and refractures. A close collaboration including clinical input, documentation, biomechanical research, and basic development allowed the AO to overcome these difficulties by defining the principles of treatment and offering thorough teaching.
From the outset less stable fixation like the more flexible version of the intramedullary nail and also external fixators, both resulting in indirect healing, were integral parts of the AO technology. But it took a long time to amalgamate observations of biological reactions to the more flexible techniques and observations relating to compression plating. As always, some ideas were not new; we mention the basic contributions to compression technology by Lambotte and Danis and those of Kuntscher to nailing. Still, to bring a new method to bear on a large scale not only requires innovative and sound ideas and ingenious individual surgical skill, but also an integrated approach to improvement and teaching to allow others to achieve similar results.
In the late eighties while studying the potential of internal fixators the team of the AO Research Institute came across a more flexible plate fixation that took advantage of locked screws. The point contact fixator (PC-Fix), which is the proof of concept of the internal fixator, was born. Animal studies showed an astonishing early solid bridging of the fractures (10 weeks) and good local resistance to infection. Furthermore, the opportunity to take advantage of monocortical threaded bolts was demonstrated. Clinical studies with exceptionally high follow-up showed low complication rates in respect to infection (Norbert P Haas, Alberto Fernandez). History repeats itself as a rule: again there were pioneers: Boitzy, Weber, and Heitemeyer (bridge plating) and we also pay tribute to Granowski (Zespol fixator). It took 40 years from the first bridge plates and nearly twenty years from successful use of the PC-Fix for the advantages of the internal fixator to be generally accepted. The difference between “me too” and leadership is rooted in basic insight and early commitment.
A new era started with great respect to biology: the era of the internal fixator. Insistence on precise reduction was replaced by restricting the aim of surgery to adequate alignment to restore the original relative positions of the two joint bearing surfaces of the long bone. Approximate alignment without touching the intermediate fragments became acceptable. The main ingredients for successful internal fixator technology still are sufficient stability for early functional treatment and, now, sufficient instability for the induction of prompt healing. The strain theory allowed definition of the degree of instability which is tolerated and the degree which induces healing.
When the bone is dead and/or infected as a result of the accident (and hopefully not of the surgery) there is a clear indication for good reduction and absolute stability and similarly precise reduction and absolute stability is a requirement for intraarticular fractures!
Living bone is able to react once it is given the chance to do so. Creating the proper biological and mechanical environment is the prerequisite. The future will show whether additional stimulation offers an advantage for fresh fractures. One may question whether stimulation will be tolerated without causing damage in desperate clinical cases such as chronic and infected nonunions. Let's not forget that it took supernatural power to revive Lazarus, in other words, I think that stimulating nearly dead cells is equally challenging.
Without perfect closure of the fracture gap it is now possible to follow the repair process within the gap radiologically. We can now pinpoint those cases that require the long-term presence of the implant to avoid refracture. Some of the observations of delayed healing are not an indication of less satisfactory healing, but they are a consequence of improved visualization.
While the LISS is a further refinement of the PC-Fix, the LCP combines a stripped version of both the LC-DCP and PC-Fix with a threaded conical locking system to reduce jamming at removal. The LCP offers a convenient way of making the transition from conventional compression techniques to the internal fixator. As the two principles of plate screws, namely, screws that press the plate to the bone and those that keeping the plate elevated are incompatible, it is advisable to exercise discipline and not to mix these principles in the same bone fragment. This is also a challenge for teaching.
In view of the basic changes brought about by the internal fixator, it is of great merit that the initial chapter of this book discusses the basics of the principles. Michael Wagner has undertaken with success the task of explaining the practical aspects of the basic concepts.
The book may be understood as a technical manual but, far more, it is offering a basic understanding. This is an important aspect in view of the fact that the implant reflects only the mechanical aspect of the realization of the internal fixator philosophy; balancing biology against pure mechanics involves the implants and the surgeons. The statement of Girdlestone “rather gardening than replacement” is up-to-date.
The second chapter of the book deals with basic clinical aspects; namely reduction of the fracture as a prerequisite to successful internal fixation. When reading this chapter one is tempted to add to Girdlestone with “rather elegant surgical technique than brute force”.
The chapters on LISS and LCP are actually technical manuals, “how to do it”. With great care the sequential steps of the internal fixation, the special characteristics of the implants and, for instance, the importance of large span bridging and attention to screw leverage using long plates are explained.
The last chapter addresses the possible errors, “what not to do” and special procedures if difficulties arise.
I hope the reader enjoys this comprehensive book—this “first shot” as much as I have done.
Stephan M Perren, Prof. Dr. med. D.Sc. (h.c.)Davos, April 2006
Contributors
Editor
Michael Wagner, Univ.-Prof. Dr. med.Facharzt für Unfallchirurgie undSporttraumatlogieWilhelminenspitalMontleartstrasse 37AT-1160 Wien
Robert FriggChief Technology OfficerSynthes BettlachGüterstrasse 5CH-2544 Bettlach
Coeditors
Richard Buckley, MD, FRCS(c)University of CalgaryFoothills Medical Center1403-29 Street N.W.CA-Calgary AB T2N 2T9
Emanuel Gautier, PD Dr. med.Hôpital Cantonal FribourgClinique de chirurgie orthopédiqueCH-1708 Fribourg
Michael Schütz, Prof. Dr. med.Princess Alexandra Hospital (PAH)2 George StreetGPO Box 2434AU-Brisbane 4001
Christoph Sommer, Dr. med.Kantonspital ChurLoëstrasse 170CH-7000 Chur
Authors
Martin AltmannSynthes BettlachGüterstrasse 5CH-2544 Bettlach
Reto Babst, Prof. Dr. med.Kantonsspital LuzernUnfallchirurgieSpitalstrasseCH-6000 Luzern 16
Hermann Bail, PD Dr. med.Klinik für Unfall- undWiederherstellungschirurgieCampus Virchow - Klinikum (CVK)Augustenburgerplatz 1DE-13353 Berlin
Peter BrunnerSynthes BettlachGüterstrasse 5CH-2544 Bettlach
Ulf Culemann, Dr. med.Klinik für Unfall-, Hand- undWiederherstellungschirurgieUniversitätsklinikum des SaarlandesKirrberger StrasseDE-66421 Homburg/Saar
Christopher G Finkemeier, MD5897 Granite Hills DriveUS-Granite Bay CA 95746
André Frenk, Dr.Synthes BettlachGüterstrasse 5CH-2544 Bettlach
Michael J Gardner, MDCornell University Medical CollegeHospital for Special Surgery535 East 70th StreetUS-New York NY 10021
Christoph W Geel, MD, FACSSuny Upstate Medical UniversityHealth Science CenterOrthopaedic Trauma550 Harrison Centre, Ste 100US-Syracuse NY 13202
Andreas Gruner, Dr. med.Unfallchirurgische KlinikStädtisches Klinikum BraunschweigHolwedestrasse 16DE-38118 Braunschweig
Norbert P Haas, Univ.-Prof. Dr. med.Klinik für Unfall- undWiederherstellungschirurgieCampus Virchow - Klinikum (CVK)Augustenburgerplatz 1DE-13353 Berlin
David L Helfet, MD, MBCHBCornell University Medical CollegeHospital for Special Surgery535 East 70th StreetUS-New York NY 10021
Thomas Hockertz, Dr. med.Unfallchirurgische KlinikStädtisches Klinikum BraunschweigHolwedestrasse 16DE-38118 Braunschweig
Keita Ito, Prof., MD, ScDAO Research InstituteClavadelerstrasse 8CH-7270 Davos Platz
Roland P Jakob, Prof. Dr. med.Hôpital Cantonal FribourgClinique de chirurgie orthopédiqueCH-1708 Fribourg
Georges Kohut, Dr. med.Hôpital Cantonal FribourgClinique de chirurgie orthopédiqueCH-1708 Fribourg
Philip J Kregor, MDVanderbilt Orthopaedic InstituteMedical Center EastSouth Tower, Suite 4200US-Nashville TN 37232-8774
Christian Krettek, Prof. Dr. med.Hannover Medical School (MHH)Carl-Neuberg-Str. 1DE-30625 Hannover
Frankie Leung, MD, FRCSQueen Mary HospitalPok Fu LamHK-Hong Kong
Wilson Li, MDDepartment of Orthopaedicsand TraumatologyQueen Elizabeth Hospital30, Gascoigne RoadHK-Kowloon, Hong Kong
Dean G Lorich, MDCornell University Medical CollegeHospital for Special Surgery535 East 70th StreetUS-New York NY 10021
Marc Lottenbach, Dr. med.Hôpital Cantonal FribourgClinique de chirurgie orthopédiqueCH-1708 Fribourg
Ingo Melcher, Dr. med.Klinik für Unfall- undWiederherstellungschirurgieCampus Virchow - Klinikum (CVK)Augustenburgerplatz 1DE-13353 Berlin
Erika J Mitchell, MDVanderbilt Orthopaedic InstituteMedical Center EastSouth Tower, Suite 4200US-Nashville TN 37232-8774
Thomas Neubauer, Dr. med.UnfallchirurgieWilhelminenspitalMontleartstrasse 37AT-1160 Wien
Stephan M Perren, Prof. Dr. med.D.Sc. (h.c.)Senior Scientific AdvisorDischmastrasse 22CH-7260 Davos Dorf
Michael Plecko, MDUnfallkrankenhaus GrazGöstingersstrasse 24AT-8021 Graz
Tim Pohlemann, Prof. Dr. med.Klinik für Unfall,- Hand- undWiederherstellungschirurgieUniversitätsklinikum des SaarlandesKirrberger StrasseDE-66421 Homburg
Heinrich Reilmann, Prof. Dr. med.Unfallchirurgische KlinikStädtisches Klinikum BraunschweigHolwedestrasse 16DE-38118 Braunschweig
Daniel A Rikli, Dr. med.UnfallchirurgieKantonsspital LuzernSpitalstrasseCH-6000 Luzern 16
Thomas P Rüedi, Prof. Dr. med., FACSAO InternationalClavadelerstrasse 8CH-7270 Davos Platz
Christian Ryf, MDClinic for Surgery and OrthopaedicsDavos HospitalPromenade 4CH-7270 Davos Platz
Klaus-D Schaser, Dr. med.Klinik für Unfall- undWiederherstellungschirurgieCampus Virchow - Klinikum (CVK)Augustenburgerplatz 1DE-13353 Berlin
Robert Schavan, Dipl.-Ing.Barschbleek 8DE-47877 Willich
James P Stannard, MDUniversity of Alabama atBirminghamDivision of Orthopaedic Surgery950-B Faculty Office Tower510 20th Street SouthUS-Birmingham AL 35294-3409
Michael D Stover, MDLoyola University Medical CenterDepartment of Orthopaedic Surgery2160 South 1st AvenueUS-Maywood IL 60153
Gabriele Streicher, Dr. med.Unfallchirurgische KlinikStädtisches Klinikum BraunschweigHolwedestrasse 16DE-38118 Braunschweig
Norbert Südkamp, Prof. Dr. med.Universitätsklinik Freiburg i.Br.Klinik für Unfall- undWiederherstellungschirurgieHugstetterstrasse 55DE-79106 Freiburg i.Br.
Hobie D Summers, MDLoyola University Medical CenterDepartment of Orthopaedic Surgery2160 South 1st AvenueUS-Maywood IL 60153
Ronald J van Heerwaarden, MD, PhDSint MaartenskliniekHengstdal 3NL-6522 JV Nijmegen
Hans Zwipp, Prof. Dr. med.UniversitätsklinikumCarl Gustav CarusKlinik für Unfall- undWiederherstellungschirurgieFetscherstrasse 74DE-01307 Dresden
Introduction
Michael Wagner
From the very outset, the goal of the Arbeitsgemeinschaft für Osteosynthese (AO) has been to improve the treatment of fractures and their sequelae. The AO proposed this by restoring integrity to the broken bone and providing the patient with early and pain-free restoration of function. The emphasis has never been solely on bone union, but has always included restoration of function—as implied in the AO's motto “Life is movement, and movement is life.”
“Fracture disease” was an obstacle to healing and mobility, and its symptoms often emerged after prolonged external splinting, immobilization in traction—consisting of chronic edema, soft-tissue atrophy, severe osteoporosis, thinning of the articular cartilage, severe joint stiffness, and sometimes chronic regional pain syndromes. Fracture disease prevented patients from starting active exercise at an early stage and delayed the return of function after bone healing. The innovative techniques introduced by the AO to combat this condition had to meet high demands. Fracture reduction had to be anatomical, and the fixation had to be stable enough to eliminate pain and allow functional rehabilitation of the limb without the risks of secondary displacement, delayed union, nonunion, or deformity. The stability produced by the compression method of fracture osteosynthesis met these requirements; it was possible to start rehabilitation immediately after the operation, and most plaster immobilization techniques became outdated.
The issues that have played an important role in stimulating progress have been,
1) differentiating between the biological requirements of articular and long bone fractures;
2) greater recognition of the importance of the type and timing of treatment;
3) specific assessment of injury to the soft-tissue envelope;
4) and attention to the patient's individual functional and physiological requirements.
It is now accepted that absolute stability is mandatory only for joint fractures and some related fractures—and then only when it can be achieved without damage to the blood supply and soft tissues. Fixation of the diaphysis should always take account of length, alignment, and rotation of the limb, and the methods of choice are splinting with an intramedullary nail or an internal fixator to promote union through callus formation.
If plate osteosynthesis is required, techniques of minimal access and fixation are able to minimize insult to the blood supply to the bone fragments and adjacent soft tissue. The fixation of articular fractures requires anatomical reduction and absolute stability to enhance the healing of articular cartilage and make early motion possible so that good ultimate function will ensue. The current principle of preserving the blood supply needs to be applied at every stage of fracture management—from initial planning to consolidation. The choice of strategy and implant depends on the biological and functional demands of the fracture and should be compatible with them.
Anatomy, stability, biology, and mobilization are still the four fundamental AO principles today. However, the implications of these principles have changed in response to the findings constantly emerging from scientific investigations and clinical observations. Progressive changes in approaches and methods have been based on continuing laboratory and clinical research, with new discoveries leading to the development of many new implants and instruments. The strategy of fracture fixation with different principles, methods and techniques of internal and external fixation are dynamic, and fürther advances will continue to be made.
The AO principles
AO principles THEN
Fracture reduction and fixation to restore anatomical relationships.
Stability through fixation with compression or splinting, as required by the fracture pattern and the injury.
Preservation of the blood supply to the soft tissues and bone through careful handling and gentle reduction techniques.
Early and safe mobilization of the area being treated and of the patient as a whole.
These concise principles still embody the AO philosophy of patient care. In today's approach, the emphasis is still very much on the fact that maintaining the blood supply to the soft tissues and bone is the most important aspect of fracture care—so that the principles could also be restated as follows:
AO principles NOW
Atraumatic reduction and fixation techniques are mandatory. Reduction of long bones need not be anatomical, but instead should demonstrate axial alignment with respect to length and torsion in the diaphysis and metaphysis. Anatomical reduction is mandatory for intraarticular fractures to restore joint congruency.
Appropriate stability of the construct has to be established. Joint surfaces require anatomical reduction with absolute stability; the majority of diaphyseal fractures can be treated with methods that provide relative stability (eg, intra-medullary or extramedullary splinting).
Atraumatic soft-tissue technique should be used with appropriate surgical approaches.
Early active mobilization of the patient is expected as the fixation construct is stable enough to allow postoperative functional care.
A comprehensive classification of long bones has helped make treatment outcomes predictable. Neither the principles nor the approaches have changed, but definitions have become more refined in relation to the different methods and techniques of fracture fixation.
The revolution is continuing today—the principles remain the same, but the methods and techniques are continually developing and implants are being modified and newly invented. Today, the AO develops sophisticated scientific and technological instrument sets that lend themselves to applications that go beyond fracture treatment. This includes the treatment of complications related to fracture care, and more recently the treatment of degenerative diseases, deformations, and defects, the problems that are becoming increasingly prevalent in the aging population (such as osteoporosis).
There has been a progressive evolution in nailing and plating:
Nailing
From conventional to locked intramedullary nailing, and
from reamed to unreamed nailing.
Plating
From very stable (absolutely stable) fixation to flexible (relatively stable) fixation, and
from compression plate fixation to locked internal fixation.
The AO principles
AO principles THEN
Influences through clinical experiences and experimental investigations
AO principles NOW
1. Anatomical, precise reduction
Applied science concerning:
– bone healings,
– blood supply through soft tissue and bone,
– biological shortcomings of ORIF in multifragmentary shaft fractures lead to a new way of thinking.
As a consequence, indirect reduction techniques were developed
Fracture reduction and fixation to restore anatomical relationships. Reductions need not be anatomical but only axially aligned in the diaphysis and the metaphysis. Anatomical reduction is required for intraarticular reductions. The principles of articular fracture care:
- atraumatic anatomical reduction of the articular surfaces,
- stable fixation of the articular fragments, and
- metaphyseal reconstruction with bone grafting and buttressing apply today as they did at the beginning.
2. Rigid fixation, absolute stability
The most notable change in the treatment of diaphyseal fractures has been the shift from the mechanical to the biological aspects of internal fixation.
The preservation of the viability and integrity of the soft-tissue envelope of the metaphysis has been recognized as the key to success.
Today the dominant theme in the fixation of fractures of the diaphysis is the biology of bone and the preservation of the blood supply to bony fragments, and no longer the quest for absolute stability.
Major changes have occurred in the timing of the different steps of metaphyseal reconstruction, as well as in the fixation methods and techniques.
The comprehensive classification of long bones has helped predict treatment and outcome.
Stabilization with different grades of stability, from high (absolute stability) to low (relative stability).
Appropriate construct stability. Stability by compression or splinting, as the fracture pattern and the injury require.
The joint surfaces require anatomical reduction with absolute stability. The majority of diaphyseal fractures are treated with relative stability methods (eg, intramedullary or extramedullary splinting).
3. Preserving blood supply
The present concept still emphasizes that the blood supply through the soft tissues and bone is the most important aspect in fracture care:
– atraumatic soft tissue technique through the appropriate surgical approaches,
– atraumatic reduction and fixation techniques are mandatory,
– implants with new bone-implant interface.
Preservation of the blood supply to soft tissues and bone by careful handling and gentle reduction techniques and a newly designed bone-implant interface.
4. Early protective motion for rehabilitation because pain was abolished and union assured
Early and safe mobilization of the part and the patient. Early active motion can also be carried out because splint fixation is stable enough to allow postoperative functional care.
Progressive evolution is the result of a long-term collaboration between the AO Research Institute (ARI), the AO Development Institute (ADI), and the Synthes manufacturers. This manual provides details of the principles and techniques involved in internal fixation using the recently developed less invasive stabilization system (LISS) and the locking compression plate (LCP). Future developments will need to address the shortcomings of the current techniques and equipment and to assess the side effects of new techniques, as well as ways of promoting healing in cases of chronically infected, atrophic nonunion. The techniques of internal fixation will also need to be fürther simplified to improve both safety and ease of handling, benefiting the treating surgeon and the patient.
Suggestions for further reading
Müller ME, Allgöwer M, Willenegger H (1965) Technique of internal fixation of fractures. Heidelberg: Springer-Verlag.
Müller ME, Allgöwer M, Willenegger H (1979) Manual of internal fixation. Heidelberg: Springer-Verlag.
Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br; 84(8):1093–1110.
Schatzker J (1998) M.E. Müller—on his 80th Birthday. AO Dialogue; 11(1):7–12.
Schenk R, Willenegger H (1964) [On the histology of primary bone healing.] Langenbecks Arch Klin Chir Ver Dtsch Z Chir; 308:440–452.
Acknowledgments
This book represents a logical step in publications from the AO. It is some years since the development of internal fixators and initial clinical experience has now been gained so that the time has come to meet the need for a book on this subject. As we become more sensitive to the specific requirements of adult learning, an important insight has been to recognize the educational value of a case-based learning program. In the light of this, we have devised an approach to describing the management of fractures that is based on a series of clinical cases submitted by different authors worldwide.
The editors would like to acknowledge and express their thanks to all the colleagues who contributed their texts and clinical cases. Their names are given in the following list:
We wish to express our full appreciation to our coeditors, Richard Buckley, Emanuel Gautier, Michael Schutz, and Christoph Sommer, who played an essential role in the production of this manual on LISS and LCP by writing, reviewing and refining the contributions. We thank them for taking on this great responsibility and giving their valuable time to this project.
Martin Altmann (Concepts)
Reto Babst (6.1.3, 6.3, 6.3.3, 6.3.4, 9.2.6, 9.2.7)
Hermann Bail (10.3.8)
Peter Brunner (Concepts)
Ulf Culemann (8.1.3, 8.1.4)
Christopher G Finkemeier (5.1.1, 5.2.2)
Andre Frenk (Concepts)
Michael J Gardner (6.1.4, 6.3.2, 7.2.4, 7.3.3, 9.1.2, 10.1.1, 10.3.5)
Emanuel Gautier (7.2.2, 8.1.1, 8.1.5, 9.1, 9.1.6, 9.2.1, 9.3.5)
Christopher W Geel (7.1, 7.1.4, 10.1.8, 10.3.4)
Andreas Gruner (7.1.6, 8.1.2, 9.2.4, 9.2.8, 9.3.2, 9.3.8, 10.1.6, 10.1.9, 10.2.12, 10.3.2, 10.3.9)
Norbert P Haas (10.3.1, 10.3.8,
David L Helfet (6.1.4, 6.3.2, 7.2.4, 7.3.3, 9.1.2, 10.1.1, 10.3.5)
Thomas Hockertz (7.1.6, 8.1.2, 9.2.4, 9.2.8, 9.3.2, 9.3.8, 10.1.6, 10.1.9, 10.2.12, 10.3.2, 10.3.9)
Keita Ito (Concepts) Roland P Jakob (9.1.6)
Georges Kohut (7.2.2)
Philip J Kregor (9.1.3, 9.1.4, 9.3.7, 9.3.9)
Christian Krettek (Concepts)
Frankie Leung (6.1.7, 10.2.4)
Wilson Li (6.1.2)
Dean G Lorich (6.1.4, 6.3.2, 7.2.4, 7.3.3, 9.1.2, 10.1.1, 10.3.5)
Marc Lottenbach (9.2.1)
Ingo Melcher (10.3.1)
Erika J Mitchell (9.1.3, 9.1.4)
Thomas Neubauer (Concepts)
Stephan M Perren (Foreword)
Michael Plecko (6.1, 6.1.8, 6.3.1, 7.1.2)
Tim Pohlemann (8.1, 8.1.3, 8.1.4)
Heinrich Reilmann (7.1.6, 8.1.2, 9.2.4, 9.2.8, 9.3.2, 9.3.8, 10.1.6, 10.1.9, 10.2.12, 10.3.2, 10.3.9)
Daniel A Rikli (7.3, 7.3.1, 7.3.5, 7.3.6)
Thomas P Rüedi (Foreword, 7.2, 10.2, 10.3)
Christian Ryf (6.1.9, 7.1.2, 7.3.2, 10.1.4, 10.2.11, 10.2.13, 10.3.1)
Klaus-D Schaser (10.3.1)
Robert Schavan (Concepts)
Michael Schutz (6.3.5, 7.1.1, 7.1.3, 9.2.3, 9.3, 9.3.6, 10.1.7)
Christoph Sommer (5.1, 5.1.4, 5.1.5, 5.2, 5.2.1, 6.1.1, 6.2, 6.2.2, 6.2.3, 6.2.4, 6.2.5, 6.2.6, 7.1.5, 9.3.3, 9.3.4, 10.1.2, 10.1.3, 10.1.5, 10.1.11, 10.2.6, 10.2.7, 10.2.8, 10.2.10, 10.3.3, 10.3.6)
James P Stannard (6.1.5) Michael D Stover (10.3.7)
Gabriele Streicher (7.1.6, 8.1.2, 9.2.4, 9.2.8, 9.3.2, 9.3.8, 10.1.6, 10.1.9, 10.2.12, 10.3.2, 10.3.9)
Norbert Sudkamp (6.1.6)
Hobie D Summers (10.3.7)
Ronald van Heerwaarden (9.3.10)
Michael Wagner (5.1.2, 5.1.3, 6.2.1, 6.2.7, 7.2.1, 7.2.3, 7.3.4, 9.1.1, 9.1.5, 9.2, 9.2.2, 9.2.5, 9.2.9, 9.3.1, 10.1, 10.1.10, 10.2.1, 10.2.2, 10.2.3, 10.2.5, 10.2.8, 10.2.9, 10.2.14, 10.2.15, 10.2.16, 10.3.10, 10.3.11)
Hans Zwipp (11)
In addition, we give a special acknowledgment to Stephan M Perren for his reviews and his foreword, to Thomas P Rüedi for supporting the project and for his foreword, to Chris L Colton for revising the extensive glossary, and to Chris G Mo-ran for ensuring the high quality of a whole range of impressive illustrations of the surgical approaches.
Apart from the contributors and coeditors, a number of people have contributed to the production of this publication. To mention them by name is only a very small token of thanks for much hard work. Hanna Jufer and her team of illustrators reliably produced high quality drawings on schedule that fully meet our expectations. Design and layout work was initiated by Sandro Isler, whereby we benefited from his vast experience.
The creation and production of a work of this magnitude has required the dedication of a number of collaborators from AO Publishing and AO International. These include Miriam Uhlmann, who was solely responsible for coordinating the project and all those involved, and for ensuring the detailed processing of the contributions, Roger Kistler, who had the task of adjusting and finalizing the overall layout, and Doris Straub Piccirillo, Urs Ruetschi, and Andy Weymann for their specialist input and valuable support.
The time and effort invested in this project has led to a most rewarding result.
Michael Wagner, Robert Frigg
Concepts
1 Background and methodological principles
1 Osteosynthesis
2 Concepts of fracture fixation
3 Mechanical aspects of plate and screw fixation
4 Development of internal fixators
5 Methods and techniques in plate osteosynthesis
6 Minimally invasive plate osteosynthesis (MIPO)
7 Bibliography
2 Surgical reduction techniques
1 Aim of reduction
2 Different types of surgical reduction
3 Instruments and techniques
4 Assessment of reduction
5 Conclusions
6 Bibliography
3 Techniques and procedures in LISS and LCP
1 The less invasive stabilization system (LISS)
2 The locking compression plate (LCP)
3 Bibliography
4 Pitfalls and complications
1 Implant-related problems
2 Technical errors
3 Pitfalls and complications during rehabilitation
4 Suggestions for further reading
1 Background and methodological principles
1 Osteosynthesis
1.1 Treatment of diaphyseal fractures: background and concepts
1.2 Treatment of articular fractures
1.3 The patient and the injury
2 Concepts of fracture fixation
2.1 Principles: absolute versus relative stability
2.2 Methods: compression versus splinting
2.3 Bone healing
3 Mechanical aspects of plate and screw fixation
3.1 General considerations
3.2 Plates and screws as compression tools
3.3 The plate as a splint
4 Development of internal fixators
4.1 History of internal fixators
4.2 Locking head screws (LHS)
4.3 The less invasive stabilization system (LISS)
4.4 The locking compression plate (LCP)
5 Methods and techniques in plate osteosynthesis
5.1 Plate osteosynthesis today and future developments
5.2 Compression method–conventional plating technique
5.3 Splinting method
6 Minimally invasive plate osteosynthesis (MIPO)
7 Bibliography
1 Osteosynthesis
The goals of fracture care are to achieve union, alignment, and function.
The general indications for fracture fixation are:
To save life or limb.
To reconstruct displaced articular fractures.
To prevent deformity.
To promote union when this is delayed.
Improved function following early motion.
The most obvious indication for operative and functional treatment is an intraarticular fracture where displacement will result in loss of function. Certain diaphyseal fractures require internal fixation: the forearm because it is a “joint” and the femur because immobilization of the injured thigh musculature will lead to a stiff, weakened leg.
Fixation of an unstable pelvic fracture, with hemodynamic instability, may be life saving. In addition, stabilization of multiple long-bone fractures may reduce mortality in patients with polytrauma.
Limb saving is another major indication. With vascular and neurological injury, the bone must be stabilized to protect the repaired structures. In open fractures, stabilization will support the soft-tissues healing.
To assure union and prevent deformity is another major reason for internal fixation. The inabilities to reduce a fracture, or maintain reduction, are indications for internal fixation.
Fractures at high risk of not healing are also ideal for surgery. Finally, internal fixation is also used in bone reconstruction for nonunion and malunion.
1.1 Treatment of diaphyseal fractures: background and concepts
Historically, internal fixation has been used as a last resort to achieve fracture union. Union has always been important and function has been a lesser concern. However, this approach to fracture treatment often sacrificed function leaving a stiff and poorly functioning extremity. At the beginning of AO history almost each fracture was stabilized with the compression method after open direct anatomical reduction. However, a problem arose: The blood supply to bone was neglected as the endeavor for perfect anatomical reduction resulted in increased tissue trauma. The perception that stable fixation was necessary led to significant damage to blood supply, increasing the rate of nonunion, infection, and failure.
The development of locked intramedullary nailing confirmed that a multifragmentary diaphyseal fracture did not necessitate an anatomical reduction. With general alignment and relative stability, union could occur rapidly. This led to the development of indirect reduction techniques: If the soft tissues were protected and biological, diaphyseal fixation techniques were used, the fracture would heal with acceptable alignment and function. Ganz, Mast, and Jakob reintroduced indirect reduction methods and biological fracture fixation solutions, eg, bridge plating (Boitzy, Weber).
Research continued on bone and its blood supply. An understanding of healing in different mechanical situations led to the strain theory of Perren. Modifications of implants to provide more stability and early function, while maintaining blood supply to the bone, such as the LC-DCP, LISS, and locking compression plates (LCP) were developed.
Current concepts still emphasize the utmost importance of blood supply to the soft tissues and bones in fracture care. The AO Principles have not changed other than that the treatment of diaphyseal and metaphyseal fractures have been refined and defined with regard to mechanics, biology, and techniques:
Atraumatic soft-tissue technique through appropriate surgical approaches.
Atraumatic reduction and fixation techniques are mandatory. Reduction need not be anatomical but axial alignment is essential (in the diaphysis and the metaphysis).
Appropriate construct stability. The majority of diaphyseal fractures are treated with relative stability techniques.
Early active motion can be carried out because fixation is stable enough to allow functional aftercare.
Precise anatomical reduction of the diaphysis in the femur, tibia, and humerus is not necessary. Function is not diminished as long as length, rotation, and axial alignment are restored. The radius and the ulna are exceptions to this rule. Pronation and supination, as well as normal elbow and wrist function, depend upon the preservation of the normal anatomical shape and relationships of the two bones. Anatomical reduction of these two bones is mandatory, and stability should be achieved with an appropriate technique.
In the following sequences some important technological innovations and conceptual changes of fracture fixation are discussed.
Locked intramedullary nailing
The development of this technique showed that diaphyseal fractures do not require precise anatomical reduction, but only correct alignment and relatively stable fixation (with intramedullary splinting of the fracture zone). This resulted in rapid union through callus formation (indirect bone healing). This led to the view that indirect reduction techniques can be used to spare the soft tissues and that flexible biological fixation techniques can be used successfully in diaphysis [1, 2].
With the emphasis today on the preservation of the blood supply to the bones and soft tissues, the locked intramedullary nail has become the implant of choice for the fixation of diaphyseal fractures [3]. Locked nailing can be performed by a minimally invasive approach. Although multifragmentary fractures used to be a contraindication to nonlocked nailing, they are currently the principal indication for the use of a locked intramedullary nail. Locked nailing has also made it possible to stabilize fractures in the proximal and distal thirds of the diaphysis, as well as to treat subtrochanteric fractures with involvement of the lesser trochanter and ipsilateral fractures of the shaft and neck of the femur [4, 5]. The new generation of locked nails extends the indications towards the proximal and distal ends of the diaphysis.
From direct to indirect reduction
Interfragmentary compression requires predominantely open direct anatomical reduction. It has been recognized that direct manipulation of bone fragments, as was usual during internal fixation procedures, was a major cause of devitalization of the bone fragments [6] (see chapter 2; Tab 2-1). In order to minimize damage to the vascularization of the osseous tissue and the surrounding soft tissues, indirect reduction techniques have become popular with open reduction and internal fixation. This approach was advocated by Mast and colleagues [7] who introduced indirect reduction methods and biological solutions such as bridge plating for diaphyseal fracture fixation.
One example of an indirect reduction method is the distraction of fragments using a distractor, an external fixator, a plate, or traction applied to a limb. The fragments are reduced using ligamentotaxis (Tab 1-1) [8–10], minimizing the extent to which they are manipulated and preserving their blood supply.
Tab 1-1
Ligamentotaxis
Ligamentotaxis is the principle of molding fracture fragments into alignment as a result of tension applied to a fracture by the surrounding intact soft tissues.
Preservation of the blood supply
Historically, the most notable development in the treatment of diaphyseal fractures has been a shift away from the mechanical aspects of internal fixation toward the biological aspects. The focus in the fixation of diaphyseal fractures today is on the biology of the bone and on preserving the blood supply to the bone fragments. A quest for absolute stability is no longer the primary aim [2, 11].
Limits of compression plating: “stress protection”
It was observed in earlier clinical and laboratory studies that the cortex under the fixation plate became excessively porous due to a marked increase in the number of haversian canals [12]. This phenomenon was explained by Wolff's law of bone remodeling (Tab 1-2), and it became known as “stress protection.” However, on investigating the biological effects of conventional compression plates on the underlying cortex, Perren and colleagues [13] made the important discovery that plates interfere significantly with the blood supply to the underlying cortex. The “stress protection” hypothesis was thus found to be mistaken. This led to the development of limited contact plates later to noncontact plates.
Tab 1-2
Wolff's law
Bones develop the structure best suited to resisting the forces acting on them. Any changes in either the form or function of a bone are followed by specific changes in its internal architecture and secondary alterations in its external shape–changes usually involving responses to alterations in weight-bearing stresses (form follows function). This applies only to long lasting unloading.
Wave plate and bridge plate
Imaginative thinking led to the development of the wave plate [14] and the bridge plate [15, 16]. The basic idea is to leave the fracture zone and its fragments undisturbed, by fixing the plate to the intact part of the bone on the proximal and distal sides of the fracture zone.
There are two advantages when a wave plate is used to bridge a comminuted fracture area. Firstly, when a plate is applied at a distance from the bone, it allows better perfusion of the repair tissue—with the benefits of better leverage and mechanical support from the repair tissue [17]. Secondly, when the plate spans an extended fracture area, there is more uniform deformation of the inner part of the plate that is not fixed to the bone—preventing the development of sites of excessive deformation that could lead to fatigue failure.
The technique of bridge plating (splinting method with plates) was developed to help prevent devitalization of fragments in multifragmentary fractures [6, 18]. The fracture is first reduced by means of indirect reduction. The fragmentation zone is then bridged with a plate that is fixed to the main proximal and distal fragments. This maintains length, rotation, and axial alignment. This type of internal fixation is a form of splinting. It is not absolutely stable, and union occurs through callus formation. This plating technique is mainly indicated for the fixation of multifragmentary fractures. If a simple transverse or oblique fracture is closely reduced and plated, thenabsolutestabilityhastobeachievedusinginterfragmentary compression; otherwise failure is likely to follow due to excessive strain at the fracture site. Clinical experience with locked plates has shown that close indirect reduction and splinting of simple fracture is possible and leads to indirect fracture healing but sometimes to a delayed bone healing.
Bone grafting
The techniques of indirect reduction and bridge plating have made bone grafting unnecessary in multifragmentary diaphyseal and metaphyseal fractures [6]. Bone grafting is now largely reserved for metaphyseal defects in articular fractures and for open fractures with bone loss.
Plates with limited bone contact
Plates having a smaller surface area in contact with the bone, even when they are thicker and more rigid, were found to cause less interference to the blood supply of bone [25]. A smaller surface contact area with the bone also leads to less intense osteoporosis than where plates which are thinner and more elastic but have a larger surface contact area with the bone. The porosis appeared to be directly related to the amount of necrosis occurring below the plate (Gautier). This observation led to the development of plates that ensure limited contact between the bone and implant, such as the limited-contact dynamic compression plate (LC-DCP).
Biological internal fixation
This approach represents the culmination of recent research, following fundamental revision of the principles of fracture fixation and conceptual and technological innovations [3, 26] (Tab 1-3). There is now a better understanding of the way in which fractures heal, and the all-important role played by the soft tissues has been recognized. As our understanding of the ways in which bones and implants interact has also improved, the importance of maintaining the vital balance between stabilization and biological function has been grasped, and biological internal fixation has been developed in order to take this into account. The principle of biological internal fixation consists of minimizing the biological damage caused by indirect reduction, the surgical approach, and by contact between the implant and the bone [2, 27]. Minimizing such damage can be achieved, but it implies less precise reduction and a less stable, more flexible fixation.
More than 100 years ago, Lane (1856–1938) first advocated the manipulation of tissues using special instruments and a “no-touch technique,” as he realized that bone healing depended as much on the condition of the soft tissues as on optimal mechanical conditions. Today's concept of biological internal fixation is based on achieving a balance between stability and biological integrity. The principle of biological internal fixation consists of minimizing the biological damage caused by the surgical approach and reduction technique by anchoring the implant only in the main fragments. The minimization of trauma is achieved at the expense of less precise reduction and less stable fixation (Tab 1-4).
Indirect reduction and pure internal splinting (based on the principle of relative stability) help keep bone fragments vital. Indirect bone healing leads to early and reliable solid union. This approach can be successful whenever the accident has not resulted in complete avascularity in the bone fragments. Still complete avascularity require fracture fixation with absolute stability.
Tab 1-4
Biological internal fixation with different implant systems
Implant
Method of fracture fixation
Position of splint
external fixator
external
locked splinting
locked nail
internal intramedullary
locked splinting
locked internal fixator
internal extramedullary
locked splinting
Tab 1-4 Biological internal fixation with the method of locked splinting using three different implant systems according to the principle of fracture fixation with relative stability.
Three main conventional techniques are available to achieve biological internal fixation: 1) splinting stabilization with external fixators; 2) splinting stabilization with intramedullary locked nails; and 3) the use of plates as pure splints—ie, without the additional lag screw effect.
With external fixators, the transcutaneous infection route offsets the positive effects of minimizing implant-bone contact and flexible fixation.
Using an intramedullary nail allows a minimally invasive percutaneous approach, but the advantages of this are somewhat offset by the extensive damage caused to the intramedullary circulation, as well as local and general intravascular thrombosis due to tissue damage and possible fat intravasation caused by the high intramedullary pressure during reaming and insertion of the nail.
Splinting the fracture zone with a plate. The pioneering technique today is the locked internal fixator (locked noncontact plate) applied using a minimally invasive technique. Research and development in this area are ongoing, and further modifications and improvements with this method can be expected in the near future.
From absolute to relative stability
The method of compression fixation using lag screws and conventional plates (based on the principle of absolute stability) has therefore been supplemented by the method of splinting (based on the principle of relative stability), taking advantage of pure splint fixation with a plate [6]. The latter method provides flexible fixation that stimulates callus formation and consequently promotes early solid union.
The less invasive stabilization system (LISS) and locking compression plate with locking head screws (LCP with LHS) now incorporate the methodological principles of locked internal extramedullary splinting [28]. LISS and LCP with LHS resemble plates but act biomechanically as locked splints or fixators—locked internal fixators (LIF).
1.2 Treatment of articular fractures
The principles of the treatment of articular fractures are the same today as they have always been:
Atraumatic anatomical reduction of the articular surfaces
Stable fixation of the intraarticular fragments
Reconstruction of the metaphysis with bone grafting and buttressing by bone grafting and buttress plate
Functional postoperative treatment without immobilization
What has changed is the sequence of the different steps of metaphyseal reconstruction.
Intraarticular reconstruction must be undertaken as early as possible and with the least possible trauma to the tissues. Any delay leads to permanent deformity, as the articular fragments unite rapidly and defy later attempts at reduction. Intraarticular cartilage does not remodel [29]. Any residual incongruity becomes permanent and can lead to posttraumatic arthritis. In contrast, the diaphysis and metaphysis have a tremendous capacity for remodeling and any residual deformities can be relatively easily corrected by osteotomy.
The timing of articular and metaphyseal reconstruction and the techniques used are vital therefore. It has been recognized that preserving the viability and integrity of the soft-tissue envelope of the metaphysis is the key to success. External fixation is therefore often used as a temporary measure, to establish the length and alignment of the metaphysis, with definitive reconstruction being delayed for 2–3 weeks until the soft-tissue envelope has recovered [30, 31]. If the articular fragment or articular bone block is small and does not provide any purchase for an external fixator, then the joint is bridged temporarily to provide the necessary immobilization.
Whether final reconstruction is carried out as a primary procedure or as a delayed procedure, every possible step is taken to minimize damage to the blood supply to the soft tissue and bone. The measures required for this include indirect reduction, minimal exposure, and percutaneous screw fixation of the fragments. Buttressing is still important in preventing axial deformity, but buttressing techniques are now designed to minimize soft-tissue trauma. Buttressing can now be achieved by plating, by using an angular stable plate-screw construct such as a blade plate.
1.3 The patient and the injury
General and local factors affecting management decisions
It is important to identify the patient factors that will effect treatment, to look at the preoperative risk factors, and to identify other factors of the injury that may change the treatment plan. Patient assessment is best done through the preoperative history and physical examination as well as by various investigations that are required to determine the health of the patient and the presence of blood born pathogens. Informed consent must include a discussion of the expectations of treatment between the patient and the surgeon.
The injury itself has both systemic and fracture-associated effects. The systemic effects involve the multiple trauma patients. Fracture-associated concerns are soft-tissue injury, particularly a crush syndrome or fractures causing fat embolism, or vascular and nerve injury. The role of the soft tissue in healing, infection, and function is important and influences the timing and type of fixation. The treatment objectives of the soft-tissue injury are first to maintain tissue perfusion, to prevent necrosis, to avoid infection, and to prevent further damage of any soft tissue. This is best done by stabilizing the soft tissues to promote healing and function and ultimately to promote bone union. This is accomplished by skeletal stabilization, which decreases the injury inflammatory response and bacterial spread while increasing perfusion and promoting wound repair. The choice of fixation technique is based upon the principle that insult to biology is to be minimized while mechanical stability must allow early function. Thus, a balance must be achieved between the amount of surgical biological insult necessary to achieve stabilization, the degree of instability and the mechanical stability necessary to allow early function and to induce callus to achieve union.
Timing
Fracture surgery is emergency, urgent, or elective. Emergency surgery is immediate for life and limb-threatening problems. Where as urgent surgery occurs within 12 hours, elective can usually be booked leisurely after 24 hours and is a planned intervention with the optimized patient and surgeon.
Patient preparation will be determined by the particular nature of the injury and patient condition. Elective surgery will allow a proper case history to be completed to determine comorbidities and assessment of risks in order to optimize the outcome. An optimal plan for fracture care should exist including plans for appropriate postoperative care determined with the patient. Patients who require urgent surgery can usually be optimized, as most of this surgery is done to prevent complications such as infection in open fractures by debridement but patient understanding of the severity and consequences of the injury will be limited.
The final aspect is emergency surgery, and this is time-dependent based on the injuries present such as hemorrhage, vascular insufficiency, head injury, or other associated injuries requiring emergency life-saving intervention. It may be to save a life or a limb and little can delay it, but may also be at a point where the whole concept of limb salvage is impossible due to the fact that the patient is too ill and requires expedient surgery. This is a specific example where orthopedic trauma care supersedes fracture care thus modifying it in relation to the patient condition. This is the multiply injured patient.
Injury assessment and conditions will modify any treatment as evidenced by the multiply injured patient, but preoperative plan and tactic must include the patient and the associated injury as well as the fracture.
Ultimately the timing of surgery is not determined by the fracture but by the patient's physiological condition and soft-tissue injury. The preoperative plan allows the surgeon to go through the proposed operative fixation procedure, and so to identify potential problems before they occur. It is a visualization of the process and techniques that may be necessary to perform the reduction and fixation.
2 Concepts of fracture fixation
The theoretical principles underlying fracture fixation are the establishment of the concept of stability—absolute or relative stability meaning maximal or less mechanical stability after the osteosynthesis. The two methods applied in order to achieve these goals are compression (static or dynamic) or splinting (locked or unlocked). A variety of techniques and implant technologies are applied in the steps required to carry out these methods (Tab 1-5).
The present section describes the principles and methods of fracture fixation, compression and splinting, and bone healing, and the reaction of bone to implants. chapter 2 describes the general techniques used for reduction and their relation to different types of fixation. chapter 3 describes the specific techniques and procedures used for the less invasive stabilization system (LISS) and locking compression plate (LCP) technologies and the handling of the implants and instruments involved.
2.1 Principles: absolute versus relative stability
There are two main principles involved in fracture fixation— absolute stability and relative stability. Absolute stability is best achieved through interfragmental compression using the lag-screw technique. In certain situations absolute stability is achieved by plate compression. Regardless of the technique selected, the surgeon will need to obtain an anatomical reduction which restores structural continuity of the bone and provides stable fixation allowing partial weight bearing and early muscle rehabilitation of the extremity. Relative stability implies a more flexible atraumatic stabilization procedure that has the advantage of preserving blood supply [2]. The corresponding techniques can therefore be referred to as “biological internal fixation” (Tab 1-4).
The two principles of fracture fixation result from the concept of stability (Fig 1-1).
The term “stability” is used here in accordance with its meaning in clinical practice—ie, referring to the extent to which load-dependent displacement between the fracture surfaces is possible. If the fractured surfaces are compressed in accordance with the principle of absolute stability, then only minimal displacement between the fragments can occur. By contrast, if the fracture zone is splinted using implants that do not exert compressive forces, relative displacement can be proportional to the load applied and in inverse proportion to the rigidity of the splinting device which bridges the fracture.
Fig 1-1 Spectrum of stability.
Definitions
Stability is defined as the degree of displacement between fracture fragments.
Rigidity is defined as the physical properties of the implant or the ability of the implant to counter deformation. However, a rigid implant may be applied to a fractured bone in a way that is providing poor stability, ie, instability.
Stability after osteosynthesis is a spectrum from minimal to absolute. Where there is no motion between the fracture fragments, under load absolute stability exists. The second condition; relative stability, is where there is some motion between the fracture fragments. The amount of stability between fracture fragments is also determined by the degree of impaction between the fragments. This will produce intimate contact and restore structural continuity to the bone, thus restoring the load-bearing capacity to the bone (implant-bone construct shares the stresses). However, the degree of stability varies depending upon the bone contact or methodology. Healing is possible in this variable stability situation as demonstrated in the strain theory of Perren.
Strain theory